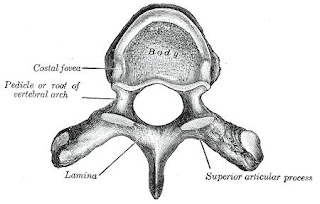
Laminectomy is an orthopaedic spine operation to remove the portion of the vertebral bone called the lamina. There are many variations of laminectomy. In the most minimal form small skin incisions are made, back muscles are pushed aside rather than cut, and the parts of the vertebra adjacent to the lamina are left intact. The traditional form of laminectomy (conventional laminectomy) excises much more than just the lamina; the entire posterior backbone is removed, along with overlying ligaments and muscles. The usual recovery period is very different depending on which type of laminectomy has been performed: days in the minimal procedure, and weeks to months with conventional open surgery.
Nursing Diagnosis for Postoperative Laminectomy, according to Doenges (1999), Tucker (1998).
1. Anxiety related to a crisis situation, continuous pain disorder.
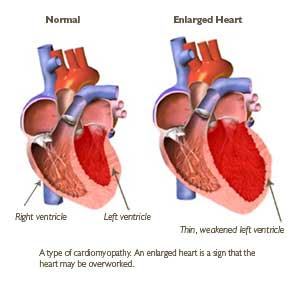
2. Ineffective tissue perfusion related to decreased blood flow secondary to edema surgery.
3. Ineffective airway clearance related to decreased lung expansion secondary to pain.
4. Pain (acute / chronic) related to physical injuries agent; compression of nerve, muscle spasm, the incision surgery.
5. Impaired physical mobility related to pain and discomfort, muscle spasm, neuromuscular damage.
6. Constipation related to immobility, decreased physical activity.
7. Knowledge deficit: the condition, prognosis and actions related to lack of knowledge or information.
Nursing Diagnosis for Postoperative Laminectomy, according to Doenges (1999), Tucker (1998).
1. Anxiety related to a crisis situation, continuous pain disorder.
2. Ineffective tissue perfusion related to decreased blood flow secondary to edema surgery.
3. Ineffective airway clearance related to decreased lung expansion secondary to pain.
4. Pain (acute / chronic) related to physical injuries agent; compression of nerve, muscle spasm, the incision surgery.
5. Impaired physical mobility related to pain and discomfort, muscle spasm, neuromuscular damage.
6. Constipation related to immobility, decreased physical activity.
7. Knowledge deficit: the condition, prognosis and actions related to lack of knowledge or information.